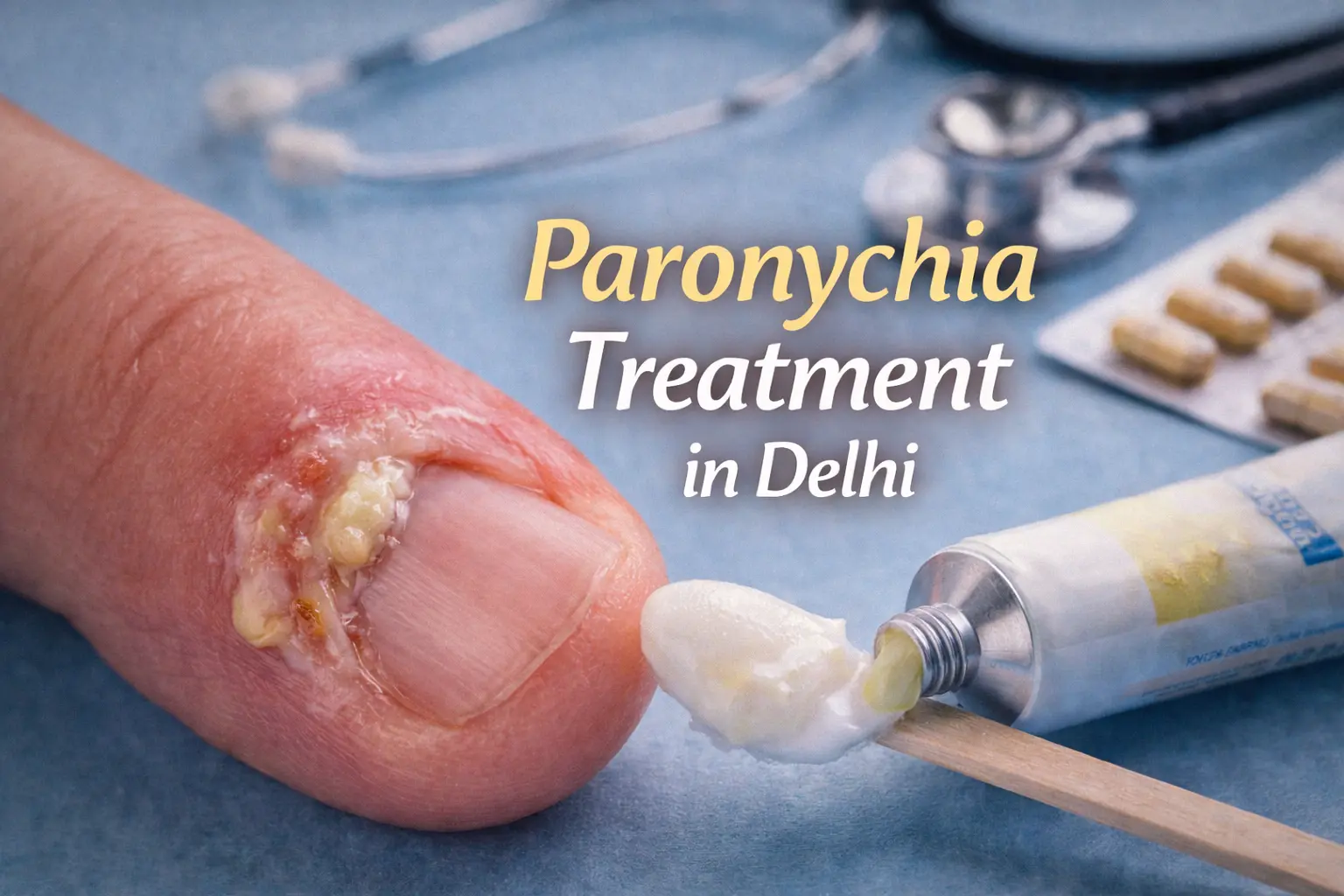
Paronychia — a painful infection around the fingernail or toenail — is common, but it doesn’t have to derail your day. Whether you’re searching for “paronychia treatment in Delhi,” “acute paronychia treatment,” “chronic paronychia treatment,” or “paronychia treatment near me”, this guide explains how to recognise the condition, what helps at home, when antibiotics or procedures are necessary, and why choosing the right clinic matters. Read on for practical advice, simple prevention tips, and clear next steps.
What is paronychia? (quick primer)
Paronychia is an infection of the nail fold (the soft tissue around the nail). It can be:
- Acute paronychia — usually bacterial, comes on quickly, and often forms a painful abscess.
- Chronic paronychia — develops slowly (weeks to months), commonly linked to repeated moisture exposure, irritants, or fungal organisms.
Symptoms include redness, swelling, tenderness around the nail, pus or discharge (in acute cases), and sometimes nail deformity if the infection persists.
Causes & risk factors (what starts it)

Paronychia starts when bacteria or fungi enter the skin at the cuticle or nail fold. Typical triggers include:
- Nail-biting, hangnails or aggressive manicure.
- Repeated wet work (dishwashing, laundry) or exposure to detergents.
- Diabetes, immune-suppression, or poor circulation.
- Pre-existing nail conditions (onychomycosis) or chronic contact dermatitis.
Because of these causes, prevention often begins with simple daily habits.
Home care & first-aid (what to try immediately)
For mild or early paronychia, you can start safe home care immediately:

- Warm soaks: Soak the affected finger/toe 3–4 times daily for 10–15 minutes in clean warm water. This soothes pain and encourages drainage.
- Keep it dry between soaks: After soaking, dry gently and keep the area clean.
- Topical antiseptic/ointment: Apply a topical antiseptic (chlorhexidine) or an over-the-counter antibiotic ointment (mupirocin or fusidic acid where available) after soaking.
- Avoid tight shoes or pressure (for toes).
- Don’t lance at home: Never try to cut or drain an abscess yourself — that risks worsening infection and scarring.
If you see improving redness and less pain within 48–72 hours, conservative care likely suffices. If symptoms worsen, seek clinical care.
Over-the-counter (OTC) and topical options
Several OTC and topical products provide symptom relief and early control:
- Topical antibiotic ointments (mupirocin, fusidic acid) — useful for localized bacterial infection.
- Topical antiseptics — chlorhexidine or povidone-iodine for cleaning.
- Topical antifungals — if chronic paronychia has a fungal component (usually combined with other measures).
- Emollients & barrier creams — for chronic cases due to wet work, to protect skin.
Always patch-test a new product and stop if irritation occurs.
When antibiotics or a procedure are needed
You should see a dermatologist if any of the following occur:
- Worsening pain, spreading redness, fever, or red streaks.
- Visible pus collection (abscess) that does not drain with warm soaks.
- Recurrent or chronic nail-fold inflammation.
- Underlying conditions (diabetes, peripheral vascular disease, immune suppression).
Acute paronychia with an abscess often requires incision and drainage performed by a clinician under sterile conditions. In addition:
- Oral antibiotics may be prescribed if infection is spreading, systemic symptoms are present, or a high-risk patient (e.g., diabetic). Common choices include oral cephalexin or amoxicillin–clavulanate for typical skin bacteria; however, the exact antibiotic depends on local resistance patterns and individual allergy history.
- Topical antibiotics (e.g., mupirocin) may suffice for small, localized infections without systemic signs.
Chronic paronychia often needs a different approach: avoid moist exposure, use topical steroids to control inflammation, treat fungal elements with topical antifungals when indicated, and correct any irritant exposures. In stubborn cases, minor surgical procedures (nail-fold debridement) or culture-guided therapy may be advised.
Important: This information outlines common approaches but does not replace a doctor’s prescription. Always consult a dermatologist before starting systemic antibiotics.
Diagnostics — what your doctor may do
Your dermatologist will examine the nail fold and may:
- Perform a point-of-care drainage for abscess (if needed).
- Take a swab or tissue sample for culture to identify bacteria or fungi in recurrent cases.
- Order blood tests if systemic illness is suspected.
- Review your medical history (diabetes, medications) and occupational exposures.
Culture-guided therapy helps when infections fail to respond to initial treatments.
Chronic paronychia — long-term management
Chronic paronychia requires a stepwise plan:
- Stop the trigger: Reduce wet work and avoid irritants (gloves for chores).
- Topical anti-inflammatory therapy: Short courses of topical corticosteroids to control inflammation.
- Antifungal therapy: If Candida or dermatophytes contribute, topical or oral antifungals may be prescribed.
- Surgical options: For long-standing deformity or persistent tissue overgrowth, a minor surgical procedure may be needed.
With correct diagnosis and consistent care, many chronic cases improve significantly.
What other clinics often miss (and what we do differently)
Many providers treat paronychia as a “one-off” problem. However, recurrent or chronic cases need a deeper approach. Common gaps include:
- No occupational assessment: Clinics often fail to investigate whether repetitive wet work or chemicals are the real cause. We get specific about daily exposures and provide realistic avoidance plans.
- No culture for recurrent infections: Without culture, antibiotic choices are blind. We test when infections recur to guide targeted therapy.
- No integrated skin-nail care: Some clinics treat the acute episode but do not manage the underlying nail/skin health. We combine medical treatment with nail-care education and protective strategies.
- Poor aftercare: Many patients are not shown safe wound care or told how to protect nails during healing; we give written aftercare and follow-up.
By addressing cause, not just symptoms, we reduce recurrence.
Why choose Sunshine Skin & Hair Clinic for paronychia in Delhi?

- Clinical expertise: Treatments are supervised by Dr. Namrata Ghai, with 21 years of dermatology experience.
- Comprehensive care: We offer safe incision & drainage, culture-guided antibiotics, antifungal therapy, and chronic-care plans.
- Diagnostic capability: On-site specimen collection, and partnerships with labs for accurate cultures.
- Affordable, transparent pricing: We provide clear cost estimates before procedures and offer staged care plans to keep costs manageable.
- Two convenient branches: South Delhi (Safdarjung Enclave) and West Delhi (Bali Nagar) for easy follow-up and continuity of care.
We focus on fast symptom relief, accurate diagnosis, and preventing recurrence.
Prevention tips — how to avoid future paronychia
- Keep nails trimmed and avoid aggressive cuticle cutting.
- Wear rubber gloves for wet work; use cotton liners if working long hours with water.
- Dry hands thoroughly after washing and use barrier creams.
- Avoid nail-biting and picking.
- Treat onychomycosis early—fungal nail disease can predispose to repeated paronychia.
- Seek early care for hangnails or small injuries.
Simple daily habits dramatically reduce risk.
People Also Ask — short answers
Paronychia: which doctor to consult?
See a dermatologist for paronychia; they specialise in nail and skin infections and can perform drainage and prescribe the right medicines.
What is the fastest way to cure paronychia?
For mild cases, warm soaks and topical antiseptics often bring quick relief. If an abscess forms, professional incision and drainage plus appropriate antibiotics give the fastest resolution.
What is the best treatment for paronychia?
Treatment depends on acute vs chronic disease. Acute infections often need drainage and antibiotics; chronic paronychia needs trigger avoidance, topical steroids and possibly antifungals.
What are the best antibiotics for paronychia?
Antibiotic choice varies by severity and local resistance. Commonly used oral agents include cephalexin or amoxicillin–clavulanate for typical skin bacteria. Topical antibiotics (mupirocin, fusidic acid) help localized infections. Always consult a doctor for prescription and allergy checks.
What is the main cause of paronychia?
The main cause is skin barrier disruption—cuts, hangnails, aggressive manicures—or prolonged moisture exposure that allows bacteria or fungi to invade the nail fold.
When to seek urgent care
Go to a clinic promptly if you have:
- Rapidly spreading redness, fever or chills.
- Increasing pain or red streaks up the finger/toe.
- Worsening despite home care.
- Diabetes or immune-suppression with any sign of infection.
Early professional care prevents complications.
Final note
Paronychia ranges from an easily managed nuisance to a persistent problem that affects daily life. For fast relief and long-term prevention in Delhi, get evaluated early. Sunshine Skin & Hair Clinic combines rapid symptomatic care with diagnostic testing and preventive strategies so you get better — and stay better.
To book an appointment or for an urgent consult, call: +91 88607 60770 (South & West Delhi branches available).
This article provides general information and does not replace medical advice. For personalised treatment, consult a dermatologist.
“`