Introduction — quick, clear guide
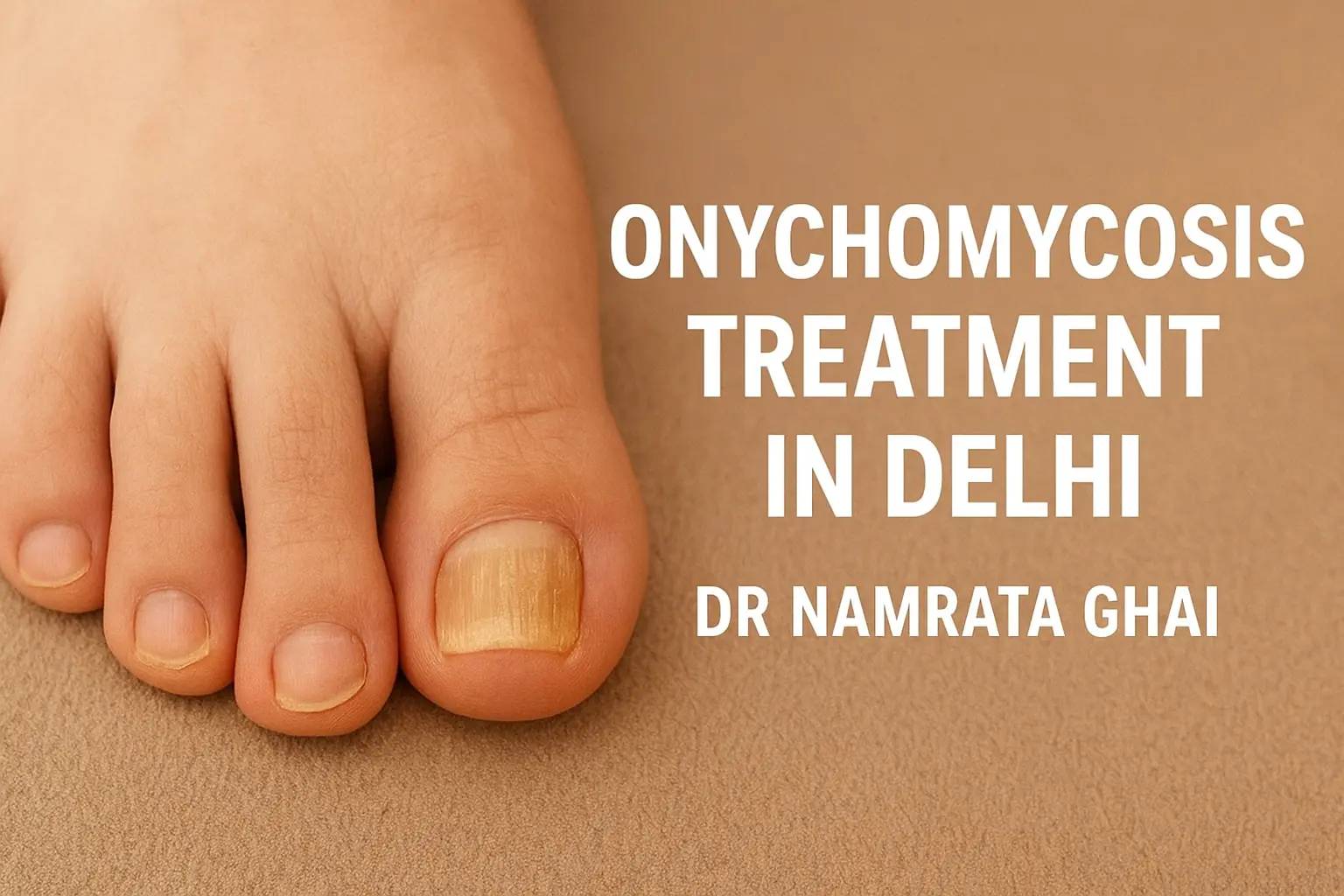
Onychomycosis (fungal nail infection) is a common cause of thick, discoloured, brittle nails. Left untreated it can spread, cause discomfort, and affect daily life. If you’re searching for onychomycosis treatment in Delhi, this guide explains what causes it, how dermatologists diagnose and treat it (medical, topical, laser), what you can safely do at home, and why choosing an experienced clinic like Sunshine Skin & Hair Clinic led by Dr. Namrata Ghai can improve results — especially for patients in South Delhi (Safdarjung Enclave) and West Delhi (Bali Nagar).
What is onychomycosis and why it happens
Onychomycosis is a fungal infection of the fingernail or toenail that commonly begins as a white or yellow spot under the tip of the nail. Over time the fungus can thicken, discolour and crumble the nail plate. Risk factors include humid conditions, nail trauma, walking barefoot in public places, diabetes, poor peripheral circulation and a weakened immune system. Proper diagnosis and targeted therapy are important, because nail fungal infections are stubborn and often need several months of treatment.
Keywords covered naturally: onychomycosis treatment in Delhi, best onychomycosis treatment in Delhi, onychomycosis treatment near me, onychomycosis treatment in South Delhi Safdarjung Enclave, onychomycosis treatment in West Delhi Bali Nagar.
How dermatologists diagnose onychomycosis
A reliable diagnosis matters because some nail problems mimic fungal infection (psoriasis, traumatic dystrophy). A dermatologist will:
- Examine the nails and surrounding skin
- Take a nail clipping or scraping for laboratory testing (microscopy/culture or rapid tests) when needed
- Evaluate contributing factors (diabetes, footwear, occupations)
Accurate lab confirmation guides therapy choice (topical vs oral vs procedural) and avoids unnecessary drug exposure.
Treatment options — what works and when
1. Topical antifungal therapy
For mild, superficial infections limited to part of the nail, prescription topical antifungals or medicated lacquers can be effective. Topicals are safe but require persistence and good nail care; they work best when the fungal infection has not invaded deep under the nail plate.
2. Oral antifungal medications
Systemic oral antifungals are often the most effective option for moderate-to-severe infections or those affecting many nails. These drugs require medical supervision and routine blood tests because of possible side effects. A dermatologist chooses the correct medication and duration based on test results and your medical history.
3. Combination therapy
Many clinics combine oral therapy with topical agents and mechanical nail care (debridement) to speed clearance and reduce recurrence.
4. Laser & device-assisted treatments
Fractional lasers and targeted light/laser devices are offered by some dermatology centres to improve nail appearance and assist fungal clearance. Laser approaches can be useful as adjuncts, especially when systemic therapy is contraindicated or for cosmetic improvement. Efficacy varies and dermatologists advise realistic expectations.
5. Mechanical nail care and debridement
Professional nail debridement (thinning of thickened nails) improves the penetration of topical medicines and reduces pain. Performed in-clinic by trained staff, it is often paired with medical therapy.
Home care & practical measures that help
While you follow medical treatment, these home steps reduce recurrence and support recovery:
- Keep feet dry and change socks often; choose breathable footwear.
- Use antifungal sprays or powders in shoes.
- Trim nails straight across and avoid aggressive at-home nail surgery.
- Avoid walking barefoot in public wet areas (pools, gyms).
- Treat athlete’s foot promptly (tinea pedis is a common source of nail infection).
- Disinfect nail tools and avoid shared pedicure equipment.
Home care helps but rarely cures established onychomycosis alone — professional treatment from a dermatologist is essential for the best results.
Common questions patients ask (people also ask-answers)
What is the best ointment for onychomycosis?
Topical medicated lacquers and prescription antifungal creams (selected by a dermatologist) are helpful for mild infections. The “best” product depends on the depth and type of infection — a clinician will recommend the appropriate topical or systemic option.
How do you fix onychomycosis at home?
At-home measures (dry foot care, antifungal powders, hygiene) help prevention and support therapy, but complete cure of established nail fungus usually needs prescription treatment under a dermatologist’s guidance.
Does onychomycosis ever go away?
Yes — with appropriate treatment (oral and/or topical therapy, good nail care and time) many patients achieve clear or improved nails. Full visible recovery may take months because new healthy nail growth is slow.
Why many clinics miss the mark — services patients should insist on
Some centers only offer topical creams or quick cosmetic fixes. For durable success, patients need:
- Proper laboratory confirmation of fungal infection (avoid trial-and-error therapy)
- A combined plan (medical + mechanical + footwear/environmental advice)
- Follow-up to monitor side effects of oral medicines and to confirm clearance
- Education on preventing reinfection
If a clinic skips lab confirmation, omits systemic options when indicated, or does not give practical relapse-prevention advice, outcomes may be poor.
Why Sunshine Skin & Hair Clinic is a smart local choice for onychomycosis in Delhi
(Please ensure these clinic details are accurate before publishing.)
- Accurate diagnosis: nail microscopy/culture or rapid tests to confirm fungus and identify species when needed.
- Personalised treatment plans: we customise topical, oral or combination therapy depending on severity and patient health.
- On-site nail debridement & laser options: professional nail trimming, thinning and laser adjuncts to speed cosmetic improvement.
- Safe monitoring: if oral antifungals are prescribed we monitor liver function and provide clear safety guidance.
- Affordable, staged care: by recommending the least-invasive effective path first and using combination care only when necessary, we often keep costs lower than centres that jump to expensive options. Negotiated supply costs and efficient care pathways also help reduce patient bills.
- Local convenience: regular follow-up clinics in South Delhi (Safdarjung Enclave) and West Delhi (Bali Nagar) so patients can complete long treatment courses easily.
How Dr. Namrata Ghai’s approach is different
Dr. Namrata Ghai brings 21 years’ clinical dermatology experience and emphasizes lab-confirmed diagnosis, sensible staged therapy, and practical relapse-prevention. Her team focuses on combining medical effectiveness with affordability and patient education — reducing unnecessary repeat visits and ensuring safe monitoring for systemic drugs.
When to see a dermatologist urgently
See a specialist promptly if you have:
- Painful, rapidly worsening nail changes
- Suspected bacterial superinfection (pus, warmth, fever)
- Underlying diabetes or circulation problems (higher risk of complications)
- Recurrent infections despite home care
Practical next steps — booking & preparation
- Photograph affected nails for baseline comparison.
- Note past treatments and any liver or kidney disease (important for oral drug safety).
- Expect treatment courses lasting many weeks to months; follow-up ensures safe and effective care.