What is epidermolysis bullosa (EB) — a short, clear explanation
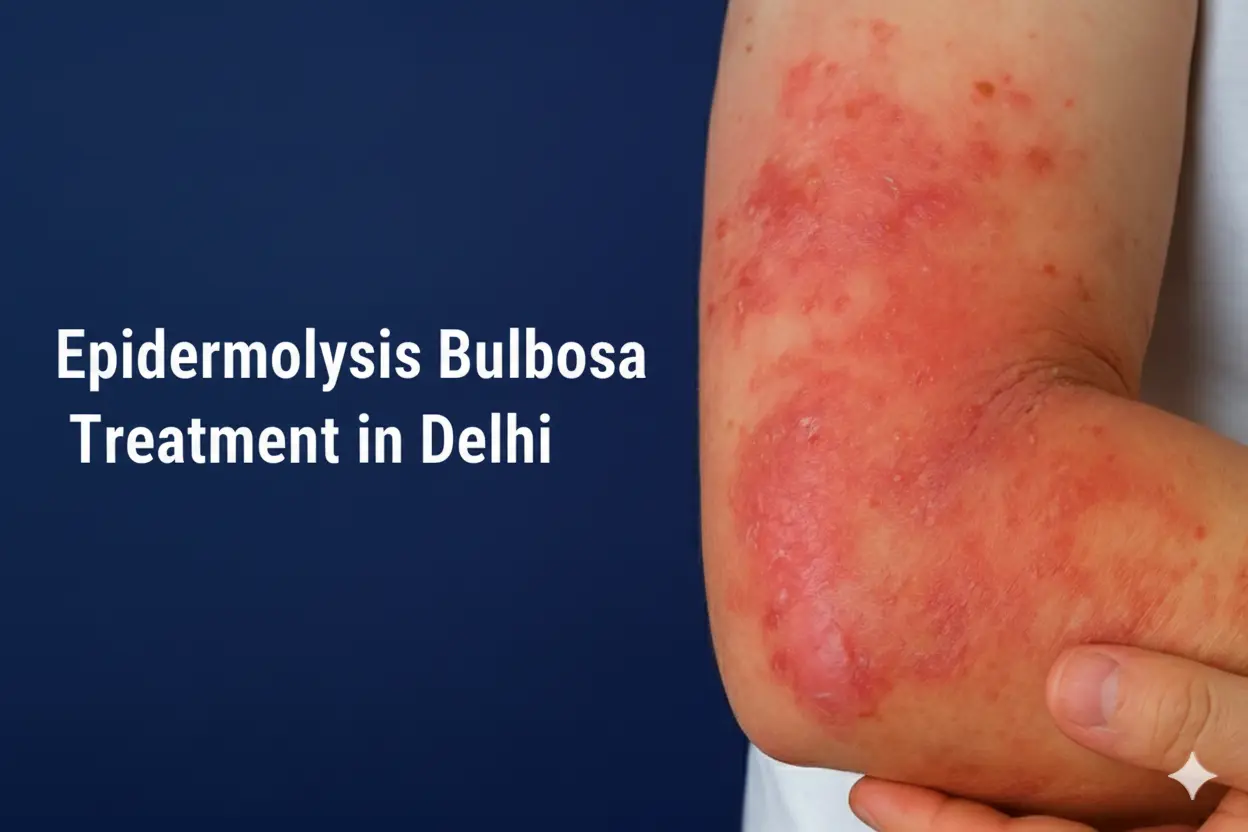
Epidermolysis bullosa (EB) is a group of inherited (genetic) skin disorders that make the skin very fragile — even small friction or minor trauma can cause painful blisters and wounds. EB ranges from mild forms to severe subtypes that affect the mouth, throat and internal tissues. Management historically focused on symptom control, wound care and preventing complications.
Why EB happens (causes & types)
EB is caused by mutations in genes that produce structural proteins responsible for holding skin layers together. Different gene defects produce different EB types (simplex, junctional, dystrophic), and severity varies by subtype. Genetic testing helps identify the subtype and guide prognosis and care.
Who treats EB — the best doctor for epidermolysis bullosa treatment
EB care is multidisciplinary. Primary specialists involved are dermatologists (often pediatric dermatologists for children), geneticists, wound-care nurses, dietitians and occasionally surgeons and dentists. For best outcomes, patients should be seen at clinics with EB experience or at specialised centres with multidisciplinary teams.
If you are searching locally, keywords such as “epidermolysis bullosa treatment in South Delhi Safdarjung Enclave”, “epidermolysis bullosa treatment in West Delhi Bali Nagar” or “epidermolysis bullosa treatment near me” will help you find teams that coordinate wound care, nutrition and specialist referrals in the Delhi area.
Current treatment landscape — what works today (and new advances)
- Supportive care & meticulous wound management remain central: non-adhesive dressings, careful cleansing, infection prevention, pain control and nutritional support. These measures dramatically improve quality of life and reduce complications.
- Multidisciplinary care (dermatology, nursing, nutrition, physiotherapy, dental) substantially improves outcomes. EB centres provide coordinated protocols and patient education.
- Recent therapeutic advances: For dystrophic EB, topical gene therapy and advanced gene/cell therapies have reached regulatory milestones in recent years — for example, Vyjuvek (a topical gene therapy) and other advanced cell-based treatments have been approved or are being rolled out in some regions to improve wound healing in certain EB subtypes. These are promising but have access, referral and cost implications.
Bottom line: while historically there was no cure for EB, emerging gene and cell-based therapies are changing the landscape for specific subtypes — but most patients still rely on expert wound care, infection control and supportive therapies today.
What to expect at a specialist appointment in Delhi
A specialist EB consultation typically includes:
- Clinical subtype assessment and documentation of blister distribution.
- Wound-care review (dressings, infection signs).
- Nutritional screening and plan (many EB patients have higher caloric needs).
- Pain-management review and medication adjustments.
- Genetic testing or review of prior genetic reports and referral to a genetic counsellor if needed.
- A tailored care plan and education for caregivers including dressing technique and infection prevention.
Home-care & immediate steps families can take (practical, evidence-based)
While specialist care is essential, families can significantly help at home:
- Gentle handling and protective clothing: soft, seamless clothing reduces friction.
- Non-adhesive dressings and correct wound cleaning: use saline/sterile water and avoid alcohol or harsh antiseptics unless instructed.
- Regular dressing changes with clean technique and prompt medical review for signs of infection (increased redness, pus, fever).
- Pain control and distraction techniques for children (appropriate analgesics as advised by your doctor).
- Nutritional support and oral care — many EB patients need calorie-dense diets and special dental attention.
- Vaccination and infection prevention according to specialist guidance.
These measures reduce complications but do not replace specialist / centre follow-up.
People also ask — short answers
What kind of doctor treats epidermolysis bullosa?
A dermatologist (often a paediatric dermatologist for children) leads care; geneticists, wound-care nurses and multidisciplinary teams also play essential roles.
Has EB been cured? Can epidermolysis bullosa go away?
There is currently no universal cure for all EB types. However, recent approvals for targeted gene and cell therapies (for select subtypes) have shown major improvements in wound healing; long-term access and effectiveness are evolving. Most EB care remains supportive and focused on wound management and complication prevention.
What is the new medication for epidermolysis bullosa?
Recent advances include topical gene therapy (Vyjuvek) and newer cell-based gene therapies that received regulatory attention in 2023–2025. These are indicated for specific EB subtypes and usually available via specialist centres. Discuss eligibility with your dermatologist.
What is the life expectancy of EB?
Life expectancy depends on subtype and severity. Some forms (mild simplex) have near-normal life expectancy; severe junctional or dystrophic forms can shorten survival and increase long-term complications. Exact prognosis is individual and improved with specialist care.
What are the symptoms of bullous skin disorder?
Symptoms include fragile skin that blisters easily, chronic wounds, nail changes, mouth and throat blisters, and pain. Severity and additional issues (e.g., scarring, strictures) depend on subtype.
How painful is epidermolysis bullosa?
EB can be very painful, particularly during blister formation, dressing changes and when wounds become infected. Pain management is a core part of care.
Things many clinics miss — what EB patients most need (and what to ask)
Many general clinics focus on wound dressing only. EB patients need:
- A coordinated care plan (wound care + nutrition + pain control + dental) — not just isolated dressing changes.
- Caregiver training for safe dressing and handling.
- Long-term surveillance for complications (scar tissue, contractures, and in some subtypes, skin cancers).
- Access to clinical trials / advanced therapies when eligible.
Ask prospective clinics whether they provide these and whether they connect patients to EB networks or clinical trials.
Why Sunshine Skin & Hair Clinic is an excellent local option for EB care in Delhi
(Use or edit these factual claims to match your clinic’s real services.)
- Multidisciplinary coordination: We coordinate dermatology, nutrition, wound nursing and surgical referrals to deliver a single, patient-centred plan — reducing travel and delays.
- Experienced leadership: Dr. Namrata Ghai (21 years of dermatology & trichology experience) leads EB care at Sunshine; she focuses on thorough assessment, family training and staged care plans for fragile-skin patients.
- Advanced wound-care protocols: we use non-adhesive dressing strategies, infection surveillance protocols and pain-management regimens tailored to EB patients.
- Access & referral for advanced therapies: we help patients access genetic testing, obtain specialist referrals for gene/cell therapeutics and guide eligibility for new treatments.
- Cost-sensitive care plans: by offering staged, pragmatic treatment pathways and negotiating supply pricing where possible, we strive to make effective EB supportive care more affordable than many large corporate centres (exact costs vary by patient needs).
- Local convenience: clinics in South Delhi (Safdarjung Enclave) and West Delhi (Bali Nagar) provide geographically convenient follow-up for Delhi families.
How Dr. Namrata Ghai’s approach differs from many dermatologists
- Long experience with fragile-skin protocols: two decades managing complex dermatology and hair disorders, with emphasis on safe procedural decisions for patients with fragile skin.
- Education & caregiver training: structured hands-on dressing workshops and printed care plans for families — most clinics do not provide this level of training.
- Patient navigation for advanced therapies: proactive support for genetic testing, documentation and arranging specialist referrals and clinical-trial pathways.
Practical next steps (call to action)
If you or a family member needs evaluation for blistering skin or suspected EB in Delhi:
- Collect recent photos and any prior pathology/genetic reports.
- Book a specialist dermatology consultation (ask for a paediatric dermatologist for children).
- Ask about wound-care training for caregivers and whether the clinic links to nutrition and pain-management services.
- If you want, contact Sunshine Skin & Hair Clinic to discuss coordinated care and practical referral pathways for advanced therapies.